25 year old female with Dengue fever
** This is an ongoing case. I am in the process of updating and editing this ELOG as and when required.
Note: This is an online E Log book recorded to discuss and comprehend our patient's de-identified health data shared, AFTER taking his/her/guardian's signed informed consent.
Here, in this series of blogs, we discuss our various patients' problems through series of inputs from available global online community of experts with an aim to solve those patients' clinical problems, with collective current best evidence based inputs.
This E-log book also reflects my patient-centered online learning portfolio and of course, your valuable inputs and feedbacks are most welcome through the comments box provided at the very end.
I have been given the following case to solve, in an attempt to understand the concept of "Patient clinical analysis data" to develop my own competence in reading and comprehending clinical data, including Clinical history, Clinical findings, Investigations and come up with the most compatible diagnosis and treatment plan tailored exclusively for the patient in question.
CASE SHEET
Chief complaint: Patient presented with chief complaints of body pains since 9 days and fever since 6 days, headache since 6 days.
History of presenting illness: Patient was apparently asymptomatic 6 days ago when she developed generalized body painsand joint pains involving the knee,ankle and metacarpophalyngeal joints, sudden in onset, aggravated on onset of fever and releived on medication.
6 days ago the patient developed fever which was sudden in onset and of high grade ranging between 101 to 104F as measured by the patient on seperate occasions. Continuous, with no diurnal variation, releived on medication.
At the onset of fever patient also developed headache which was diffuse throbbing type not associated with aura, dizziness, tinitus aggravated on raise of temperature and releived on medication.
Upon the set of fever the patient visited a local RMP who prescribed her a paracetamol for her fever and asked her to get tested for dengue.
The patient visited a diagnostic centre in Nakrekal and was reported to be NS 1 positive.
On receiving report patient came to our hospital to seek treatment for the same
On day one of admission that is 3 days ago the patient developed vomiting. She vomited 6 times within a day. The vomitus contained digested food. It was not blood tinged. No aggravating or releiving factors
The patient also complained 4 episodes of loose stools 3 days ago.
Hess test positive on day of admission
Patient had abdominal tenderness on day of admission.
It has also been noted that patient said she went to visit relatives a week ago where there were a lot of mosquitoes and she says she developed the illness ever since.
DAILY ROUTINE
Before the onset of illness patient used to wake up at 8AM and eat breakfast by 9 Am. She then did some household chores and are lunch by around 2:30. The patient has a 6 month old baby who she tends to most of the time. She has a glass of milk by 5 PM and dinner by 9 to sleep by 10 PM
Since the onset of disease patient complained of excessive lethargy but still tends to the baby and breastfeeds her regularly.
History of past illness:
No similar complaints in the past.
Not a known case of diabetes,htn, tb,asthma, epilepsy.
Drug history: Patient started taking paracetamol and antibiotics 3 days ago at onset of fever
No other treatment history
Personal history:
Appetite is reduced since onset of fever.
Mixed diet
Normal bowel and bladder movements
No sleep disturbances
No addictions and allergies.
Family history: No significant family history
Menstrual history: 30 day regular cycle with flow lasting for 6 days and usage of 2 pads per day. Bleeding is not associated with pain and clots
Obstetric history: P1L1, spontaneously conceived, full term LSCS birth to a healthy baby girl weighing 2.5 kg with no complications.
Environmental risk factors:
Patient reports that many people in her neighborhood have gotten dengue in the past few weeks.
She says she lives close to open fields and the area is clean with regular garbage disposal.
Patient beleives she acquired the disease due to a visit to relatives house 1 week back where there were excessive number of mosquitoes
General examination:
Conscious coherent and cooperative. Moderately built and nourished.
Pallor: absent
Icterus: Absent
Cyanosis: absent
Clubbing: absent
Koilonychia: absent
Lymphadenopathy: absent
Vitals:
Temperature: currently afebrile.
101 to 104 fever 6 days ago. Patient admitted 3 days ago and temperature maintained between 99 to 98 in these 3 days
Respiratory rate: 22 cpm
Pulse : 82 bpm
Blood pressure: 110/70 mm of Hg
Abdomen examination:
Inspection: Abdomen in scapohoid, all quadrants move equally with respiration.
Umbilicus inverted
Suprapubic scar present.
No visible peristalsis.
No hernial orifice
Palpation
Superficial:
tenderness in right hypogastrium and right lumbar
Tenderness in left hypogastrium and lumbar region
Tenderness in epigastrium
Hepatomegaly present
Spleenomegaly present.
No fluid thrill
Percussion: resonant note all over abdomen
Auscultation: normal bowel sounds heard
CVS examination: S1, S2 heard no murmurs
Respiratory system examination: NVBS. No adventitious sounds
CNS examination:
Higher Mental Functions intact
Normal speech and language
Memory: immediate retention and recall present, recent and remote intact
No delusions or hallucinations
Cranial nerve examination
- I : Intact bilaterally
III, IV, VI : Extraocular movements free and full bilaterally, direct , consensual and accommodation reflex present bilaterally
V : Intact bilaterally
VII:Intact bilaterally
VIII: No nystagmus, intact bilaterally
IX,X : Intact bilaterally
XII : Intact bilaterally
Motor System examination
Bulk : normal in upper and lower limbs bilaterally
Power : normal Power of
- Shoulder , Elbow , Wrist , Smalll muscle of hand and hand grip bilaterally
- Hip , knee , ankle , small muscle s of foot bilaterally
Muscle tone : normal
Reflexes: normal bilaterally
Higher functions:
Speech: Normal, coherent
Gait: normal
No signs of meningeal irritation
Laboratory investigations:
Blood sugar
Day 2
Day 4
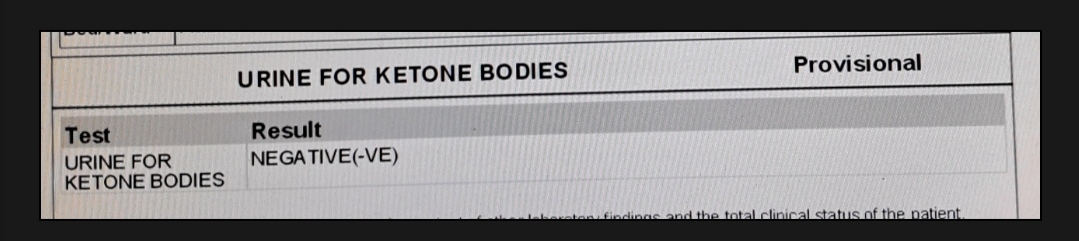
Urine ketone negative
Blood group
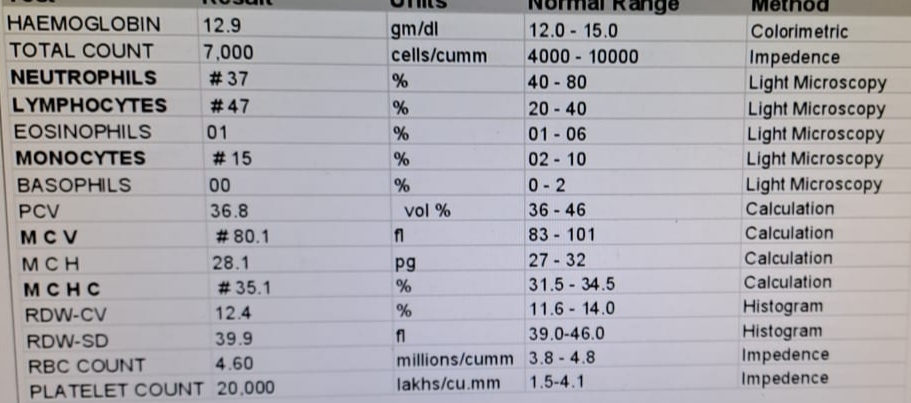
Hemogram:
Day 1
Day 2
Day 3
Day 4
Electrolytes
Day 2
Day 3
Serum creat and urea
LFT
ECG:
IMAGING: USG abdomen and pelvis
Provisional Diagnosis: Fever due to Dengue
Treatment:
Day1 : IV fluids NS @75 ml/hr
Tab. Doxycycline 100mg PO/BD
Inj. Optineuron 1 amp in 100 ml NS IV OD
Temperature 4th hourly
BP tmonitoring 2nd hourly
Inj. Zofer 4mg IV BD
Inj. Pan 40 mg OD
1 ORS sachet in 1 l water
200 ml ORS after each episode of loose stools
Day 2:
IV fluids NS @200 ml/hr
Tab. Doxycycline 100mg PO/BD
Inj. Optineuron 1 amp in 100 ml NS IV OD
Temperature 4th hourly
BP monitoring 2nd hourly
Inj. Zofer 4mg IV BD
Inj. Pan 40 mg OD
1 ORS sachet in 1 l water
Inj. PCM 1 gm IV if temp > 101F
Day 3:
IV fluids NS @200 ml/hr
Tab. Doxycycline 100mg PO/BD
Inj. Optineuron 1 amp in 100 ml NS IV OD
Temperature 4th hourly
Inj. PCM 1 gm IV if temp > 101F





























Comments
Post a Comment